Secondhand smoke and secondhand aerosol
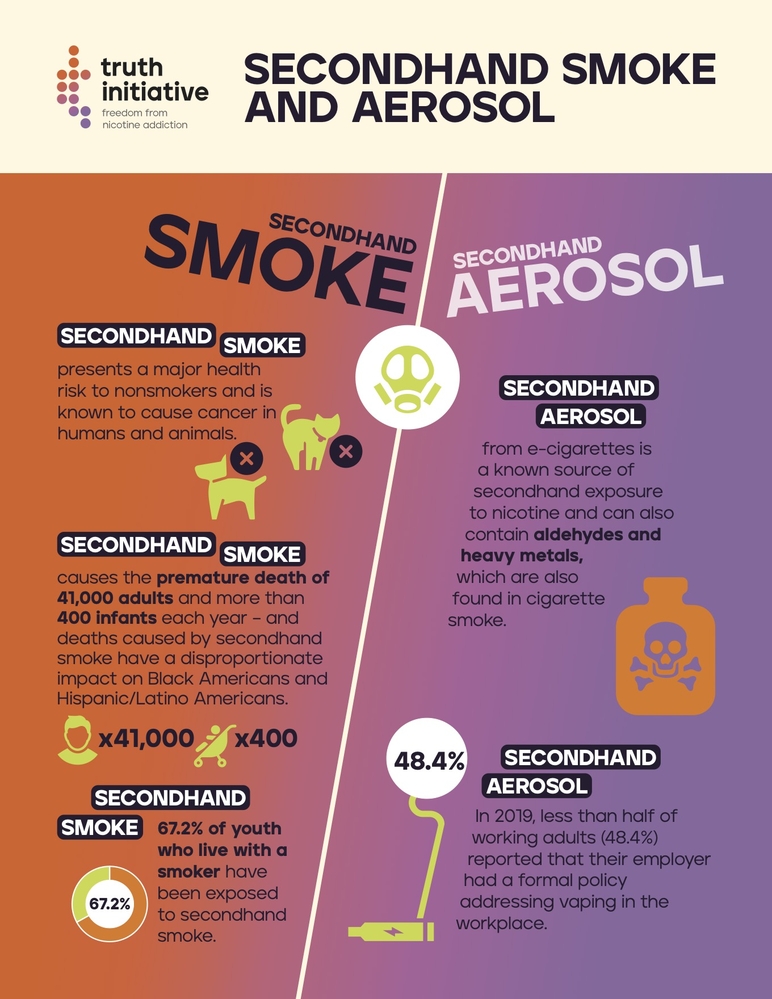
In 1986, the U.S. Surgeon General concluded that secondhand smoke was a major health risk to nonsmokers. In 2014, the Surgeon General estimated that secondhand smoke causes the premature death of 41,000 adults and more than 400 infants each year. Secondhand smoke is classified as a Group A carcinogen, a substance known to cause cancer in humans and animals.
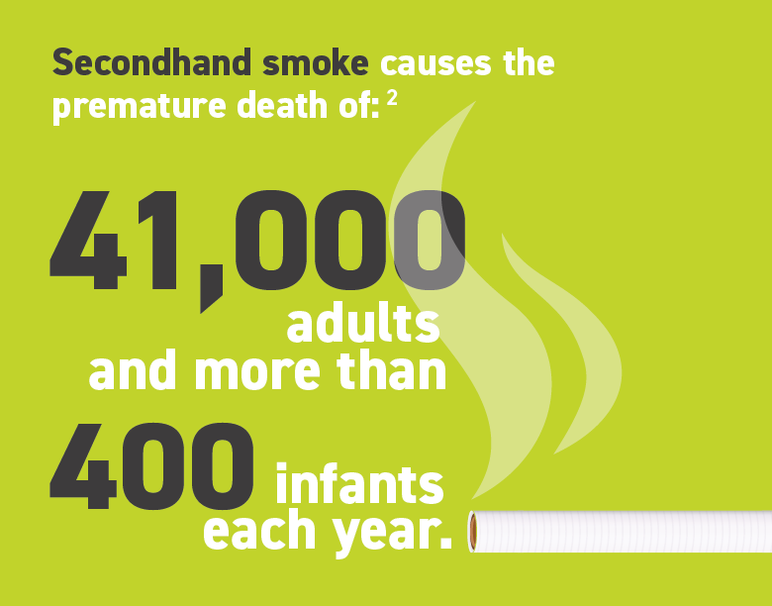
In 1986, the U.S. Surgeon General concluded that secondhand smoke was a major health risk to nonsmokers. In 2014, the Surgeon General estimated that secondhand smoke causes the premature death of 41,000 adults and more than 400 infants each year. Secondhand smoke is classified as a Group A carcinogen, a substance known to cause cancer in humans and animals.
With the rise of e-cigarettes as a popular tobacco product among young people today, secondhand aerosol exhaled by e-cigarette users presents new concerns. E-cigarette aerosol is not harmless – it contains nicotine and potentially toxic substances, according to the U.S. Surgeon General’s 2016 report on e-cigarettes. Research on the health harms of this exposure is ongoing and critical given that exposure to secondhand aerosol reported by middle and high school students rose from 24.2% to 44.5% between 2015 and 2020.
What is secondhand smoke and secondhand aerosol?
Secondhand smoke is a mixture of smoke released by the burning end of cigarettes, pipes or cigars, and smoke exhaled from smokers, which can be involuntarily inhaled by nonsmokers. Secondhand smoke contains more than 7,000 chemicals, 69 of which are known to be carcinogenic to humans or animals.
E-cigarettes heat a liquid that usually contains nicotine, flavorings, and other chemicals to create an aerosol that users inhale into their lungs. Secondhand aerosol is exhaled by e-cigarette users and exposes bystanders who are not vaping to potentially harmful chemicals. E-cigarette aerosol is made of fine and ultrafine particles at concentrations similar to those produced by cigarettes.
Below are some of the known carcinogens found in secondhand smoke:
- arsenic (used in pesticides)
- lead (formerly found in paint)
- polonium-210 (a radioactive element)
- formaldehyde (used to embalm the dead)
- benzene (a gasoline additive)
E-cigarette aerosol is a known source of secondhand exposure to nicotine and also contain the following chemicals:
- nickel (carcinogenic to humans)
- chromium (used in stainless steel)
- formaldehyde (used to embalm the dead)
- acetaldehyde (used in disinfectants)

The health effects of secondhand smoke
Due to the high number of adult and infant deaths each year resulting from secondhand smoke exposure, the Surgeon General concluded in 2006 that there is no safe level of exposure to secondhand smoke.
Infants and children
- Maternal smoking during pregnancy and exposure to secondhand smoke in infancy increases the risk of Sudden Infant Death Syndrome and contributes to low birth weight, a leading cause of infant mortality.
- Secondhand smoke can cause lower respiratory illnesses (including pneumonia and bronchitis) and persistent adverse effects in lung function during childhood. It can make children’s asthma symptoms more severe, leading to more symptomatic days and increased use of health care services, including hospitalizations.
- Research suggests a connection between secondhand smoke exposure in children and adolescents and an increased risk of developing mental health issues, such as major depressive disorder.
- Children whose parents smoke around them get more ear infections.
Adults
- Secondhand smoke exposure among nonsmokers is responsible for an estimated 7,300 lung cancer deaths and 34,000 cardiovascular disease deaths annually.
- Exposure to secondhand smoke can increase the risk of cardiovascular disease by 25% to 30% and the risk of lung cancer by 20% to 30% in nonsmokers.
- Secondhand smoke increases the risk of stroke by an estimated 20% to 30% and causes more than 8,000 deaths by stroke each year.
- Deaths caused by secondhand smoke have a disproportionate impact on Black Americans and Hispanic/Latino Americans.
- Adults exposed to secondhand smoke at home had 1.28x more hospital nights and 1.16x more emergency room visits than adults without exposure. Annual healthcare costs attributed to secondhand smoke exposure totaled $1.9 billion in 2010.
- Deaths attributed to secondhand smoke cause $6.6 billion in lost productivity per year.
Research has even shown that pets can be affected by secondhand smoke. Dogs and cats are twice as likely to develop cancer if their owner smokes, compared to animals in households without cigarette smoking.
The health effects of secondhand aerosol
Secondhand aerosol can contain harmful and potentially harmful constituents, including nicotine. A variety of potentially harmful chemicals have also been detected in e-cigarette aerosol, including aldehydes and heavy metals, which are also found in cigarette smoke. These compounds can have potential respiratory and cardiovascular effects in humans. However, there is moderate evidence that risk of secondhand exposure to nicotine and other particulates is lower from e-cigarettes compared with cigarettes, according to a 2018 report published by the National Academies of Sciences, Engineering, and Medicine (NASEM). Nonetheless, e-cigarette use degrades indoor air quality and exposes bystanders to risks associated with secondhand exposure. Indoor e-cigarette use can even set off smoke detectors.
- According to the 2018 NASEM report, there is substantial evidence that e-cigarette aerosols can induce acute endothelial cell dysfunction – a condition that typically causes chest pain. However, long-term consequences and outcomes of long-term exposure to e-cigarette aerosol are uncertain.
- Non-e-cigarette users who were exposed to secondhand aerosol had higher odds of having moderate to severe emotional and behavioral concerns such as depression, anxiety or social withdrawal, compared to non-e-cigarette users who were not exposed, according to a 2022 study.
- Among youth with asthma, secondhand aerosol exposure from e-cigarettes was associated with higher odds of reporting an asthma attack in the past year, according to the 2016 Florida Youth Tobacco Survey. Frequent exposure to secondhand e-cigarette aerosol was associated with current asthma symptoms among adolescents in Kuwait, according to a 2020 study.
Patterns of secondhand smoke and aerosol exposure
Adults and youth are exposed to secondhand smoke in places ranging from homes and vehicles to public indoor and outdoor spaces. In 2020, 12 million middle and high school students were exposed to secondhand aerosol and 16.1 million were exposed to secondhand smoke.
Smoke-free homes
- In addition to protection from secondhand smoke exposure, studies indicate that smoke-free homes and workplaces encourage smokers to quit and reduce the number of cigarettes they consume per day.
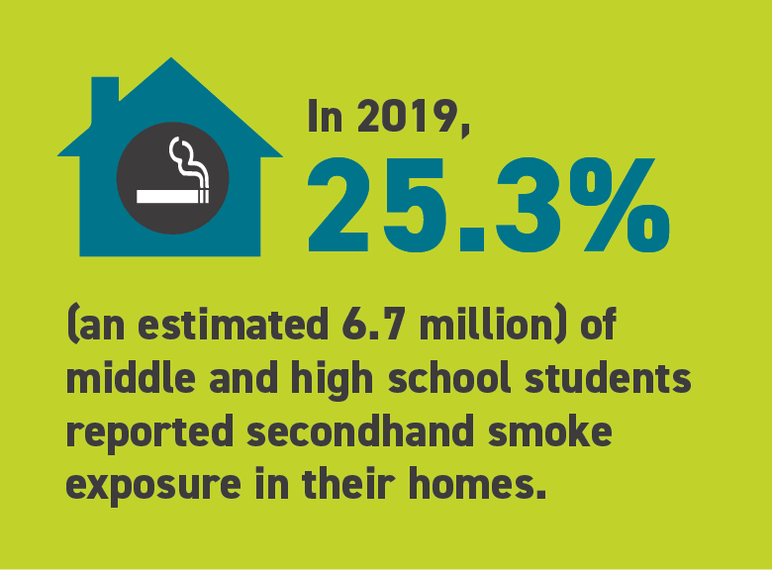
- In 2019, 25.3% (an estimated 6.7 million) of middle and high school students reported secondhand smoke exposure in their homes.
Smoking and vaping in cars
- Smoking inside vehicles can pose an even greater danger to nonsmokers because concentrations of secondhand smoke are often higher in vehicles than inside homes and bars.
- Nonsmokers exposed to secondhand smoke in cars are at an increased risk of cancer.
- Although secondhand smoke exposure in cars significantly declined from 2011 to 2018, 23.3% (6.1 million) middle and high school students reported secondhand smoke exposure in cars in 2019.
- In a study of parents who smoked cigarettes and vaped nicotine, most dual users had smoke-free home policies, yet fewer had vape-free home policies (63.8% vs 26.3%). Dual users were less likely than cigarette users to have smoke-free car, vape-free home, or vape-free car policies.
Smoking and vaping in the workplace
- The Surgeon General has concluded that comprehensive smoke-free workplace policies are the only effective means to eliminate secondhand smoke exposure in the workplace. Separating smokers from nonsmokers, cleaning the air, and ventilating buildings does not effectively eliminate exposure.
- A 2019 survey of adults employed at companies with more than 150 employees found that of employees who had seen coworkers vape nicotine in or around their workplace:
- 40.3% reported sometimes or often seeing their co-workers vape indoors.
- 40.8% sometimes or often had co-workers vape near their workspace or while conducting business with them.
- 71.6% sometimes or often saw vapor clouds from e-cigarettes.
- 52.6% sometimes or often smelled vapor from an e-cigarette at work.
- In the same 2019 survey of adult employees, nearly half of current tobacco users (46%-48%) reported workplace vaping as a trigger for their own vaping and smoking, respectively, and 7% of former users reported it as a trigger.
Smoke-free policies in the U.S.
Smoke-free legislation was associated with significantly lower rates of hospital admissions or deaths from heart attacks, heart disease, cerebrovascular accidents, and respiratory disease, according to a 2012 meta-analysis. For example, in a 2018 study of young adults, smoke-free policies in restaurants, bars, and workplaces were associated with a 24%-46% lower risk of having cardiovascular disease. In addition, cigarette smokers who were attempting to quit were predicted to have nearly two fewer smoking days per month as a result of comprehensive smoke-free laws. These findings underscore the importance of smoke- and aerosol-free policies across varied settings.
- There are few federal policies regulating smoking indoors. Federal law prohibits smoking, including the use of e-cigarettes, on flights and prohibits smoking in federal buildings.
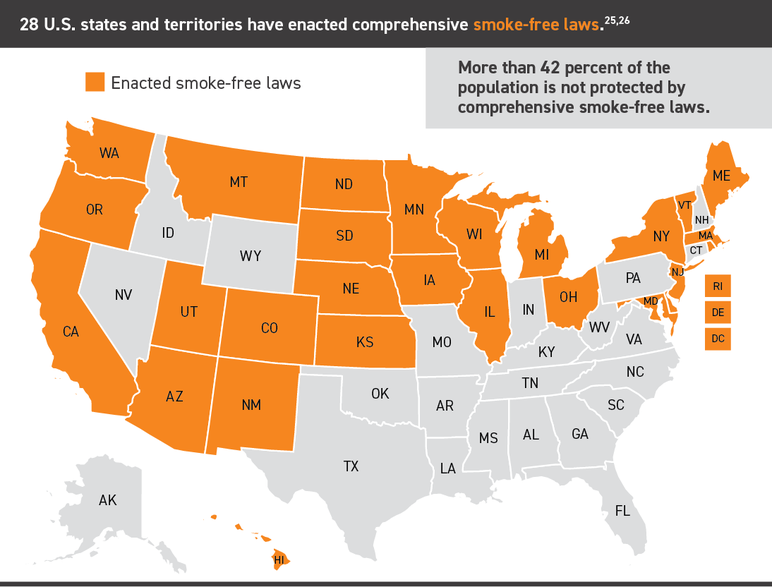
- Although 28 states plus D.C., Puerto Rico, and the Virgin Islands have enacted comprehensive smoke-free laws, disparities exist due to gaps in coverage, particularly in southern states and in places where state laws pre-empt local smoking restrictions.
- Between 1990 and 2021, national coverage of comprehensive indoor smoking restrictions increased for bars (0% to 67.3%), restaurants (0% to 78.2%), and workplaces (0% to 77.5%). From 2006 to 2021, comprehensive indoor vaping restrictions increased for bars (0% to 43.5%), restaurants (0% to 51.5%), and workplaces (0% to 53.2%). Despite these increases in coverage, by the end of 2021, less than half of the U.S. population was protected by comprehensive indoor smoking restrictions for bars (in 19 states), restaurants (in 12 states), and workplaces (in 14 states).
Workplace
- 82.4% of the U.S. population is protected by a 100% smoke-free provision in non-hospitality workplaces, and/or restaurants, and/or bars according to the American Nonsmokers’ Rights Foundation as of January 2024. Vape-free legislation is more limited, with only 26 states including e-cigarettes in their 100% smoke-free policies.
- Many workplaces do not have policies prohibiting vaping nicotine in the workplace. In a 2019 survey of U.S. employees, less than half of working adults (48.4%) reported that their employer had a formal, written policy specifically addressing e-cigarette use, 30.2% reported their employer did not have such a policy, and 21.4% did not know if they had a policy. Lack of policies persist despite overwhelming support (73%) for such policies.
Housing
- The U.S. Department of Housing and Urban Development (HUD) mandated that all public housing agencies (PHAs) adopt a smoke-free policy by July 30, 2018. The policies prohibit the use of combustible tobacco products in all indoor areas, living units and office units – and within 25 feet of these areas. As of April 2024, 84 municipalities have enacted a law at the city or county level that prohibits smoking in 100% of private units of rental multi-unit housing properties.
Vehicles
- As of April 2024, states passed laws prohibiting smoking in a vehicle when children are passengers.
College campuses
- As of April 2024, there are 2,617 colleges and universities in the U.S. with 100% smoke-free campuses.
Thirdhand smoke
- Thirdhand smoke (THS) refers to the persisting particulate matter that becomes embedded in environments exposed to cigarette smoke, even after the smoke has cleared from the air.
- Some researchers have surveyed indoor environments exposed to secondhand smoke and found multiple compounds lingering on furniture and other surfaces, such as nicotine and even carcinogenic nitrosamines.
- Additional research is needed on THS to understand the full breadth of potential health effects – especially for infants who are likely to place their mouths on objects in their environment, leading to oral exposures of THS compounds.
Action needed: Secondhand smoke and secondhand aerosol
Eliminating secondhand smoke and aerosol exposure by enacting smoke- and vape-free protections is necessary to reduce the number of deaths, illnesses, and losses of productivity that result from exposure each year.
- States and localities should pass comprehensive clean indoor air measures that prohibit smoking and vaping in all workplaces and public facilities, including restaurants, bars, and casinos, to provide protection to all people against the serious dangers of secondhand smoke and aerosol.
- E-cigarette aerosol contains many potentially toxic substances and should be included in clean indoor air laws.
- Research suggests that e-cigarette use in public places – including those designated as smoke-free such as restaurants and workplaces – could renormalize tobacco use and erode firmly established social norms that disapprove of smoking in public places. Allowing tobacco use in these spaces to once again become normalized undermines decades of efforts to the contrary.
- States and localities should enact further smoke- and aerosol-free restrictions in community settings, such as building entrances, restaurant patios, strip malls, parks, and bus stops, to reduce secondhand smoke and aerosol exposure.
- States and localities should also pass laws making multi-unit housing, such as apartments and condominiums, smoke- and aerosol-free so that secondhand smoke and aerosol does not infiltrate the units of nonsmokers.
More in harmful effects of tobacco
Want support quitting? Join EX Program
By clicking JOIN, you agree to the Terms, Text Message Terms and Privacy Policy.
Msg&Data rates may apply; msgs are automated.


